| ISSN |
| Manuscript Template |
| Make a Submission |
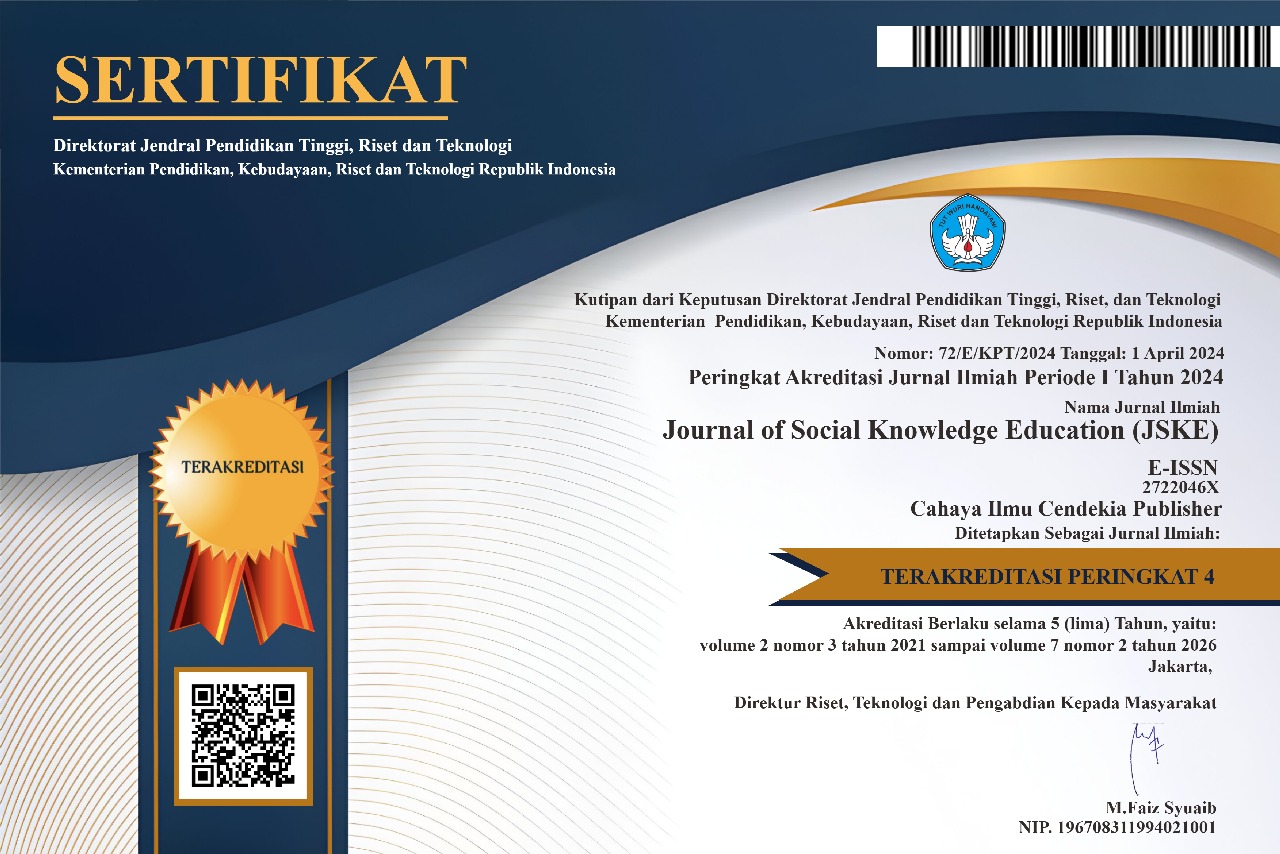
| National Accreditation |
*) Journal of Social Knowledge Education (JSKE) is Accredited SINTA 4 by the Director General of Higher Education, Research, and Technology, No. 72/E/KPT/2024| Vol. 2, No. 3, 2021 - Vol. 7, No. 2, 2026
| Publisher |
In Collaboration With
| In Partnership with |
| People |
| Editorial Team |
| Peer-Reviewers |
| Contact |
| Policies |
| Focus and Scope |
| Peer Review Process |
| Publication Ethics and Malpractice Statement |
| Publication Frequency |
| Open Access Policy |
| Repository Policy |
| Screening for Plagiarism |
| Correction and Retraction |
| Copyright and Licensed |
| Indexing and Abstracting |
| Allegations of Misconduct |
| Archiving Policy |
| Direct Marketing |
| Advertising |
| Revenue Source |
| Submission |
| Author Guidelines |
| Online Submission |
| Privacy Statement |
| Article Publication Charge |
| Information |
| For Readers |
| For Authors |
| For Librarians |
| Recommended Tools |
| Visitor |
| Indexing and Abstracting |
| Journal Metrics |
| Acceptance Rate : | 43 % |
| Review Speed : | 75 days |
| Issue Per Year : | 4 |
| Number of Volumes : | 6 |
| Number of Issues : | 21 |
| Number of Articles : | 119 |
| No. of Google Citations : | 287 |
| Google h-index : | 8 |
| Google i10-index : | 6 |
| Abstract Views : | 14,372 |
| PDF Download : | 13,600 |
UPDATE: 10 May 2025


.png)
.png)